Stomatitis is a general term that refers to the inflammation and soreness of the mouth. It can affect any part of the mouth, such as the lips, cheeks, gums, tongue, and palate. It may have various causes, such as infections, injuries, allergies, or diseases. It can also cause different types of sores, such as canker sores or cold sores. Stomatitis can interfere with your ability to eat, speak, and sleep, and it can affect your quality of life.
In this comprehensive guide, we will cover everything you need to know about Stomatitis and by the end of this guide, you will have a better understanding of what Stomatitis is, how it affects your oral health, and what you can do to manage it.
Table of Contents
Types and Symptoms of Stomatitis:
There are two main types of stomatitis: Canker Sores and Cold Sores.
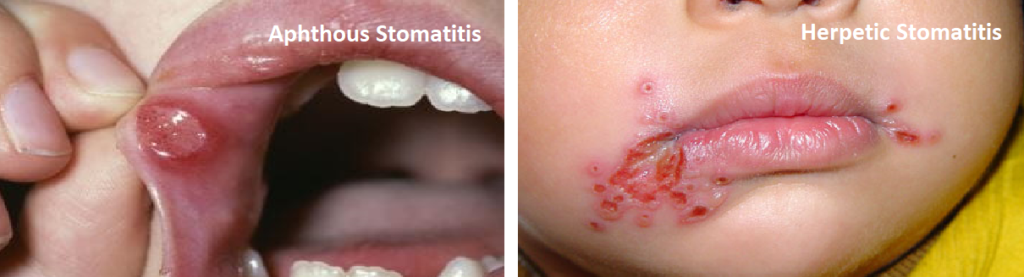
Canker sores are also known as Aphthous Stomatitis or Aphthous Ulcers, and they are small, white or yellow ulcers with a red border that appear inside the mouth. They are not contagious, but they can be very painful and make eating and drinking difficult. Canker sores usually heal within one to two weeks, but they can recur frequently.
Cold sores or Herpetic Stomatitis are also known as fever blisters, and they are caused by the herpes simplex virus type 1 (HSV-1). They are small, fluid-filled blisters that appear on or around the lips. They are contagious, especially when they burst and form a crust. Cold sores can cause tingling, burning, or itching sensations before they appear. They usually heal within seven to ten days, but they can also recur periodically.
Other Types includes:
- Cheilitis or Angular Stomatitis: inflammation of the lips and around the mouth
- Glossitis: inflammation of the tongue
- Gingivitis: inflammation of the gums
- Pharyngitis: inflammation of the back of the mouth

Symptoms of Stomatitis:
May vary depending on the type and cause of the condition, but they may include:
- Redness, swelling, or bleeding of the affected area
- Pain or discomfort in the mouth
- Difficulty eating, drinking, speaking, or swallowing
- Bad breath or altered taste
- Fever or malaise
Common Causes and Risk Factors:
Stomatitis can be caused by a variety of factors that may irritate or damage the mucous membranes of the mouth. Some of these factors are:
- Infections: viral infections (such as HSV-1), bacterial infections (such as streptococcus), fungal infections (such as candida), or parasitic infections (such as leishmaniasis)
- Injuries: trauma from biting the cheek, tongue, or lip; wearing braces or dentures; having a sharp tooth; or undergoing dental procedures
- Allergies: hypersensitivity to certain foods (such as citrus fruits, chocolate, cheese, or nuts), medications (such as antibiotics or NSAIDs), dental materials (such as amalgam fillings or latex gloves), or environmental substances (such as pollen or dust mites)
- Diseases: autoimmune diseases (such as lupus, Crohn’s disease, or Behcet’s disease), inflammatory diseases (such as Sjogren’s syndrome or lichen planus), nutritional deficiencies (such as vitamin B12 or iron deficiency), hormonal changes (such as during pregnancy or menopause), or cancer (such as leukemia or oral cancer)
- Medications: certain drugs that may cause dry mouth (such as antihistamines or antidepressants), reduce immunity (such as corticosteroids or immunosuppressants), or damage the mucous membranes (such as chemotherapy or radiation therapy)
- Lifestyle factors: smoking or chewing tobacco; drinking alcohol; consuming spicy, acidic, or hot foods; stress; poor oral hygiene; dehydration; or lack of sleep
Some people may be more prone to developing stomatitis than others due to their genetic predisposition, age, gender, health status, or environmental exposure.
Diagnosis of Stomatitis:
To diagnose, your dentist or doctor will examine your mouth and ask you about your symptoms, medical history, medications, allergies, and lifestyle habits. They may also take a swab sample from your mouth to test for infections or perform a biopsy to rule out cancer.
Treatment:
The treatment depends on the type and cause of the condition. Some common treatments are:
- Antiviral medications: for cold sores caused by HSV-1, such as acyclovir, valacyclovir, or famciclovir
- Antibiotics: for bacterial infections, such as penicillin, amoxicillin, or erythromycin
- Antifungal medications: for fungal infections, such as nystatin, clotrimazole, or fluconazole
- Anti-inflammatory medications: for reducing pain and swelling, such as ibuprofen, naproxen, or aspirin
- Corticosteroids: for severe cases of inflammation or ulceration, such as prednisone, hydrocortisone, or dexamethasone
- Topical agents: for soothing and protecting the mouth, such as gels, creams, ointments, rinses, or sprays that contain anesthetics (such as benzocaine or lidocaine), antiseptics (such as chlorhexidine or hydrogen peroxide), or coating agents (such as sucralfate or carafate)
- Nutritional supplements: for correcting deficiencies or boosting immunity, such as vitamin B12, iron, folic acid, zinc, or probiotics
- Immunomodulators: for modulating the immune system and preventing recurrences, such as azathioprine, cyclosporine, or thalidomide
In some cases, stomatitis may require surgical intervention to remove the affected tissue or to correct the underlying problem.
Prevention of Stomatitis:
Stomatitis can be prevented by avoiding or minimizing the factors that may trigger or worsen the condition. Some preventive measures are:
- Practicing good oral hygiene: brushing your teeth twice a day with a soft-bristled toothbrush and fluoride toothpaste; flossing daily; using a mouthwash; and visiting your dentist regularly
- Maintaining a healthy diet: eating a balanced diet that includes fruits, vegetables, whole grains, lean proteins, and dairy products; avoiding foods that may irritate your mouth (such as spicy, acidic, or hot foods); and drinking plenty of water
- Managing stress: engaging in relaxing activities (such as meditation, yoga, or breathing exercises); getting enough sleep; and seeking professional help if needed
- Quitting smoking and limiting alcohol consumption: smoking and alcohol can dry out and damage your mouth and increase your risk of infections and cancer
- Protecting your mouth: wearing a mouth guard if you play contact sports; using lip balm with sunscreen if you are exposed to the sun; and avoiding biting your cheek, tongue, or lip
- Treating underlying conditions: following your doctor’s advice and taking your medications as prescribed if you have any medical conditions that may affect your mouth
Home Remedies for Stomatitis:
There are also some home remedies that may help relieve the symptoms of stomatitis. Some of these are:
- Applying ice or cold compresses to the affected area to reduce pain and swelling
- Rinsing your mouth with warm salt water or baking soda solution to cleanse and soothe your mouth
- Applying honey or aloe vera gel to the sores to promote healing and prevent infection
- Chewing on licorice root or sage leaves to reduce inflammation and numb the pain
- Drinking chamomile tea or milk to calm your nerves and ease the discomfort
- Taking over-the-counter pain relievers (such as acetaminophen or ibuprofen) to reduce pain and fever
However, these home remedies are not substitutes for medical treatment. You should consult your dentist or doctor if your symptoms are severe, persistent, recurrent, or accompanied by other signs of infection (such as pus, swollen glands, or difficulty breathing).
Also read Soft Bristle Toothbrush – A Must Have for Your Oral Health
When to Seek Professional Help for Stomatitis:
Stomatitis is usually not a serious condition and often resolves on its own within a few days or weeks. However, in some cases, stomatitis can lead to complications such as:
- Dehydration: due to loss of fluids from the mouth and reduced intake of water
- Malnutrition: due to difficulty eating and absorbing nutrients from food
- Infection: due to bacteria or fungi entering the bloodstream through the open sores
- Scarring: due to damage to the mucous membranes and skin of the mouth
- Cancer: due to chronic inflammation or exposure to carcinogens
Stomatitis can also affect your emotional well-being and social life. You may feel embarrassed, depressed, anxious, or isolated because of your appearance and discomfort.
The outlook of stomatitis depends on the type and cause of the condition. Most cases of stomatitis are mild and self-limiting. However, some cases of stomatitis may be chronic and recurrent. You may need long-term treatment and follow-up care to prevent flare-ups and complications.
We hope that now you have better understanding of what Stomatitis is, how it affects your oral health, and what you can do to manage it. If you staill have any query, suggest or feedback, please post the same in comment. We would love to hear from you! 😊
Thank you.

3 thoughts on “Stomatitis : A Comprehensive Guide to Painful Mouth Sores”